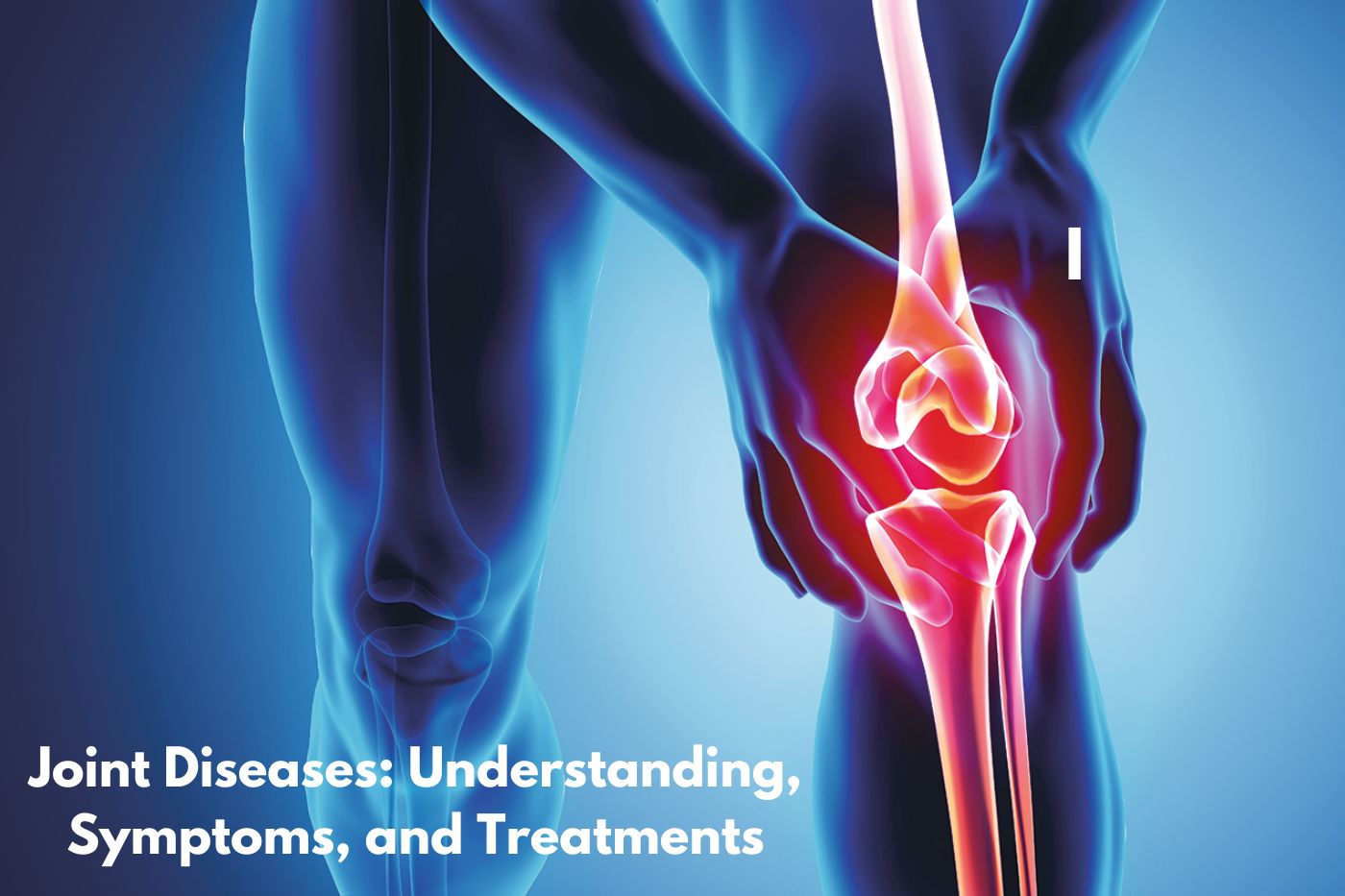
Joint diseases affect millions of people worldwide, leading to pain and reduced mobility. These conditions can significantly impact daily life, making understanding and managing them essential.
Joint diseases encompass various disorders, including arthritis, bursitis, tendinitis, and more. They may result from injuries, chronic inflammation, or autoimmune diseases. This article will explore the different types of joint diseases, their symptoms, causes, and available treatments.
The Importance of Joint Health
Joint health is crucial for overall well-being. Healthy joints allow for smooth movement and flexibility, enabling individuals to engage in daily activities. When joint problems occur, they can lead to pain, stiffness, and decreased function.
Maintaining joint health involves a combination of lifestyle choices, including diet, exercise, and proper care. Understanding joint diseases helps in taking proactive steps to protect your joint function.
Regular check-ups and awareness of risk factors can empower individuals to prevent or manage joint diseases effectively. Early intervention can make a significant difference in outcomes.
Common Types of Joint Diseases
Several types of joint diseases can affect individuals. Here are some of the most common:
- Osteoarthritis: A degenerative joint disease that causes cartilage breakdown.
- Rheumatoid Arthritis: An autoimmune disease that leads to joint inflammation.
- Bursitis: Inflammation of the bursa, causing pain and swelling.
- Tendinitis: Inflammation of the tendons, often due to overuse.
- Sprains and Strains: Injuries to ligaments and muscles around the joints.
Each of these conditions has unique characteristics and requires specific treatment approaches. Understanding these differences is vital for effective management.
Osteoarthritis: Understanding the Most Common Joint Disease

Osteoarthritis is the most prevalent form of arthritis, affecting millions globally. It occurs when the cartilage that cushions the joints deteriorates over time. This degeneration leads to pain, stiffness, and reduced mobility.
Causes and Risk Factors
Several factors contribute to the development of osteoarthritis. Age is a significant risk factor, as the likelihood of developing this condition increases with advancing years. The body naturally experiences wear and tear on the joints, making older adults more susceptible.
Obesity also plays a critical role. Excess weight adds stress to weight-bearing joints, such as the knees and hips, accelerating cartilage breakdown. Maintaining a healthy weight can help reduce this risk.
Genetics can influence susceptibility. If there is a family history of osteoarthritis, individuals may be more prone to developing it. Additionally, previous joint injuries can lead to early onset of osteoarthritis.
Symptoms of Osteoarthritis
Common symptoms include joint pain, especially after movement. Individuals may notice increased discomfort during or after physical activity. This pain can become a barrier to engaging in everyday tasks.
Stiffness is another hallmark symptom, particularly noticeable in the morning or after sitting for extended periods. This stiffness often subsides with movement but can be quite pronounced after inactivity.
Swelling in the affected joints is also common. This swelling occurs due to inflammation and can contribute to a feeling of warmth in the joint. Recognizing these symptoms early can facilitate timely management.
Treatment Options for Osteoarthritis
Treatment for osteoarthritis focuses on managing symptoms and improving joint function. Medication is often the first line of defense. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation.
Physical therapy is another effective option. A skilled therapist can design an exercise program to strengthen the muscles around the joint, improving stability and function. Stretching exercises can also enhance flexibility.
In some cases, more invasive treatments may be necessary. Surgery, such as joint replacement, may be considered for severe cases where conservative treatments fail to provide relief. Consulting with a healthcare provider can help determine the best approach.
Rheumatoid Arthritis: An Autoimmune Perspective
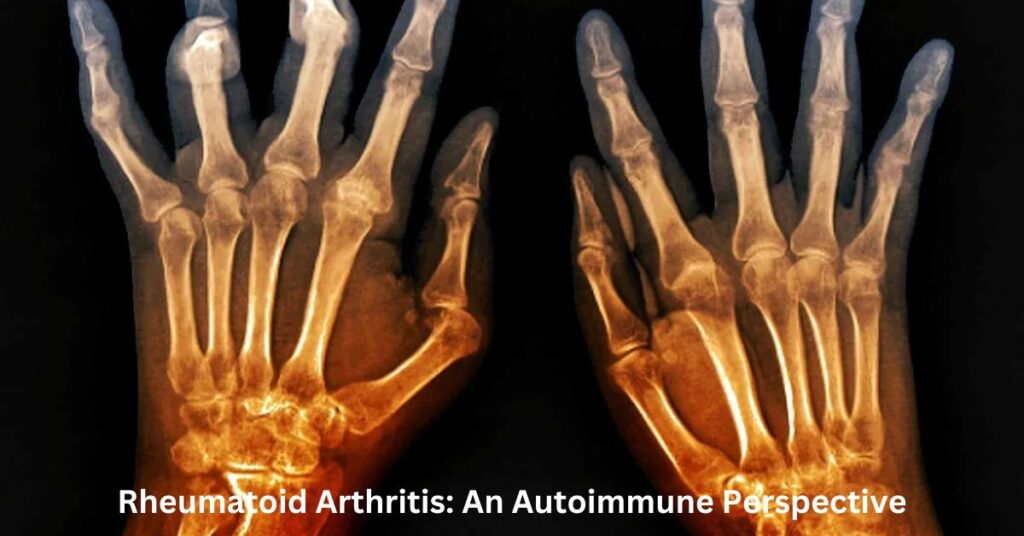
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by joint inflammation. Unlike osteoarthritis, which is primarily due to wear and tear, RA results from the immune system attacking the synovium, the lining of the joints.
Causes and Risk Factors
The exact cause of rheumatoid arthritis remains unclear. However, genetics play a significant role, as individuals with a family history of RA are at a higher risk. Environmental factors, such as smoking and exposure to certain infections, may also trigger the disease.
Hormonal factors are another area of interest. RA is more prevalent in women, suggesting that hormones may influence its development. Understanding these factors can help in identifying at-risk individuals.
Symptoms of Rheumatoid Arthritis
Symptoms of RA often begin gradually. Early signs include joint pain and stiffness, typically affecting both sides of the body. Morning stiffness lasting more than an hour is particularly characteristic.
As the disease progresses, individuals may experience swelling and deformities in the affected joints. Fatigue and general malaise are also common, as the body’s immune response can lead to systemic symptoms.
In severe cases, RA can affect other organs, such as the heart and lungs. Recognizing these symptoms early can prompt timely medical intervention and management.
Treatment Strategies for Rheumatoid Arthritis
Treating rheumatoid arthritis involves a multifaceted approach. Disease-modifying antirheumatic drugs (DMARDs) are commonly prescribed to slow disease progression and prevent joint damage. Methotrexate is a frequently used DMARD.
Biologic agents have emerged as effective treatments for RA. These medications target specific components of the immune system, reducing inflammation and improving symptoms. Healthcare providers often tailor treatment based on individual needs.
Physical therapy plays a vital role in managing RA. Therapists can help design exercises that improve strength and joint function, enhancing overall quality of life. Regular follow-ups with healthcare professionals are crucial for monitoring disease progression.
Bursitis: Inflammation of the Bursa
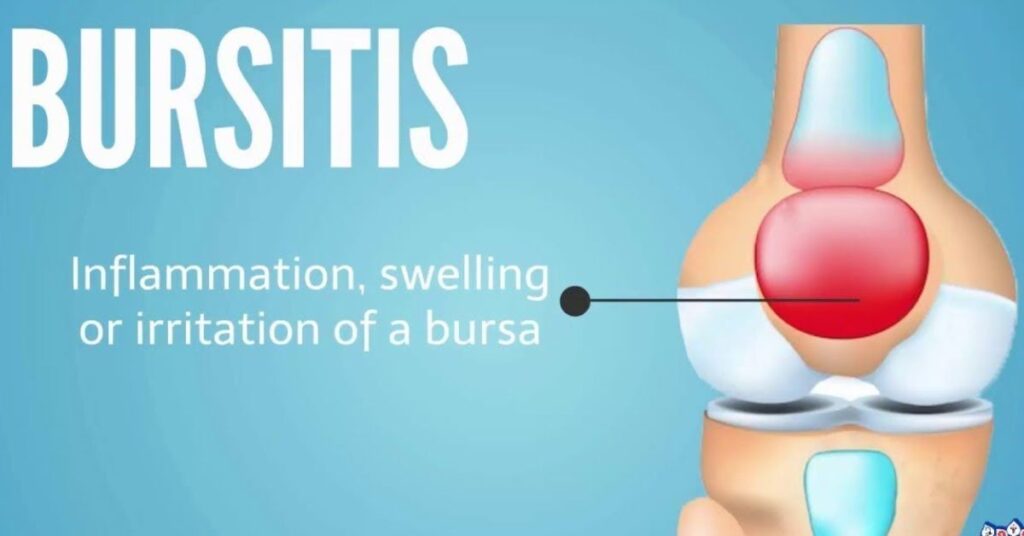
Bursitis is an inflammatory condition affecting the bursa, a fluid-filled sac that cushions joints. It often results from repetitive motions or prolonged pressure on the joint.
Causes of Bursitis
Common causes of bursitis include overuse injuries from repetitive activities, such as throwing or kneeling. Occupations or hobbies that involve repetitive motions can increase the risk.
In some cases, bursitis may develop after a joint injury or trauma. Infections can also lead to bursitis, particularly in cases of septic bursitis. Understanding the causes can help prevent recurrence.
Symptoms of Bursitis
Symptoms of bursitis typically include joint pain and swelling. The affected joint may feel tender, and movement can exacerbate discomfort. Individuals may also notice warmth or redness in the area.
Limited range of motion is another common symptom. This limitation can impact daily activities and quality of life. Recognizing these symptoms early can facilitate timely management.
Treatment Approaches for Bursitis
Treating bursitis often involves rest and avoiding activities that aggravate the condition. Ice therapy can help reduce inflammation and alleviate pain. Over-the-counter pain relievers, such as NSAIDs, may also be beneficial.
In more severe cases, healthcare providers may recommend corticosteroid injections to reduce inflammation. Physical therapy can aid in recovery by strengthening surrounding muscles and improving flexibility.
Preventing bursitis involves avoiding repetitive motions and using proper techniques during physical activities. Incorporating warm-up exercises can also help protect the joints.
Tendinitis: Inflammation of the Tendons
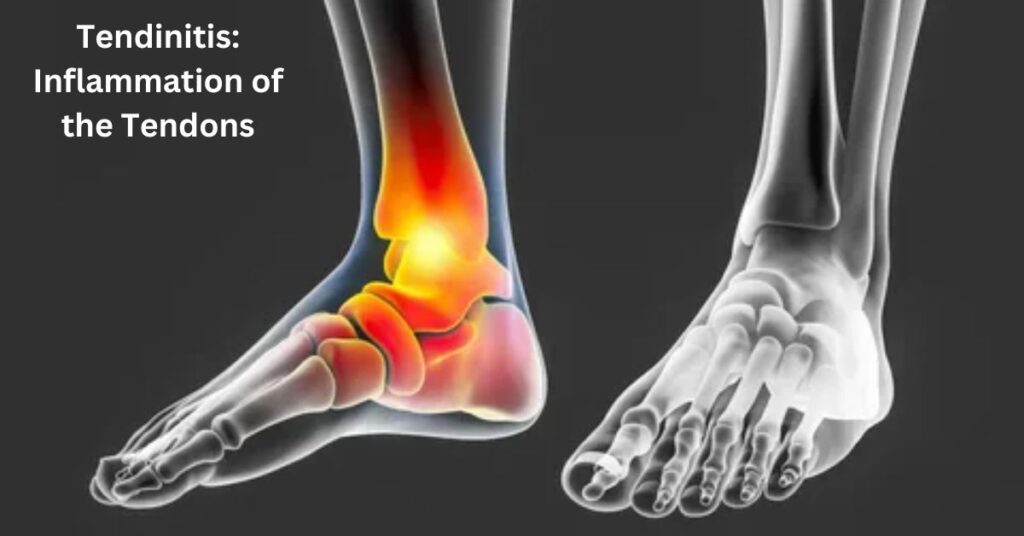
Tendinitis is characterized by inflammation of the tendons, often resulting from overuse or injury. This condition can affect various tendons in the body, leading to pain and dysfunction.
Common Causes of Tendinitis
Tendinitis is frequently associated with repetitive motions. Activities such as playing sports, typing, or manual labor can lead to tendon inflammation. Understanding these risk factors is crucial for prevention.
Age can also contribute to the development of tendinitis. As individuals age, tendons naturally become less flexible and more prone to injury. This increased susceptibility can lead to chronic tendinitis in older adults.
Symptoms of Tendinitis
Symptoms typically include tendon pain, which may worsen with movement or activity. Individuals may also experience swelling and tenderness in the affected area. A grating sensation may occur when moving the tendon.
Limited range of motion is another common symptom. This limitation can hinder daily activities, making it essential to address the condition promptly. Recognizing these symptoms early can facilitate timely intervention.
Treatment Options for Tendinitis
Treating tendinitis often involves a combination of rest and rehabilitation. Ice therapy can help reduce inflammation, while over-the-counter medications can alleviate pain. Avoiding activities that exacerbate symptoms is crucial for recovery.
Physical therapy can also play a significant role in managing tendinitis. A therapist can design a program to strengthen the affected area and improve flexibility. Gradual return to activity is vital to prevent recurrence.
In severe cases, healthcare providers may recommend corticosteroid injections or surgery. Early intervention can prevent long-term complications and ensure a successful recovery.
Read this Blog : High Cortisol Levels: Causes, Effects, and Management
Sprains and Strains: Understanding Joint Injuries
Sprains and strains are common injuries that can affect joint health. A sprain involves the ligaments, while a strain affects muscles or tendons. Both injuries can cause significant pain and limit mobility.
Causes of Sprains and Strains
Sprains often occur during activities that involve sudden stops or twists. Sports injuries, falls, or awkward landings can lead to ligament damage. Understanding these causes can help individuals take preventive measures.
Strains typically result from overexertion or lifting heavy objects. Improper lifting techniques can lead to muscle or tendon injuries. Awareness of body mechanics is crucial in preventing these injuries.
Symptoms of Sprains and Strains
Common symptoms include joint pain, swelling, and bruising. Individuals may experience limited range of motion and stiffness in the affected area. In severe cases, audible popping or tearing may occur during the injury.
Recognizing the difference between sprains and strains is essential for proper management. Prompt evaluation and treatment can help prevent complications and promote healing.
Treatment and Recovery
Treating sprains and strains often involves the RICE method: rest, ice, compression, and elevation. This approach helps reduce swelling and alleviate pain. Over-the-counter pain relievers can also provide relief.
Physical therapy may be recommended for more severe injuries. A therapist can guide rehabilitation exercises to restore strength and flexibility. Gradual return to activity is vital to avoid re-injury.
In some cases, severe sprains may require immobilization or surgical intervention. Seeking medical advice early can ensure appropriate treatment and a successful recovery.
Dislocated Joints: Recognizing and Managing Joint Dislocations
Dislocated joints occur when bones are displaced from their normal positions. This condition is often painful and can lead to serious complications if not addressed promptly.
Causes of Joint Dislocation
Dislocations typically result from trauma, such as falls, accidents, or sports injuries. Sudden impacts can cause the bones to shift out of alignment. Understanding these causes can help individuals take preventive measures.
Certain factors, such as joint hypermobility, can increase the risk of dislocations. Individuals with loose ligaments may be more susceptible to joint injuries. Awareness of personal risk factors is crucial for prevention.
Symptoms of a Dislocated Joint
Common symptoms include severe joint pain, swelling, and visible deformity. Individuals may also experience limited mobility and muscle spasms in the affected area. Recognizing these symptoms is vital for timely medical intervention.
In some cases, nerves or blood vessels may be affected, leading to numbness or tingling. Prompt evaluation is crucial to prevent complications and ensure proper treatment.
Treatment and Recovery for Dislocated Joints
Treatment for dislocated joints typically involves reduction, or realigning the bones. This procedure is performed by a healthcare professional and may require sedation for severe cases.
Following reduction, immobilization is often necessary to allow healing. Physical therapy can aid in restoring strength and flexibility. Gradual return to activity is essential to prevent recurrence.
In some cases, surgery may be required for recurrent dislocations or associated injuries. Early intervention can ensure successful recovery and minimize long-term complications.
Final insights
Understanding joint diseases is essential for maintaining overall health. Early recognition of symptoms can lead to timely intervention and effective management. Joint diseases can significantly impact quality of life, making awareness and prevention crucial.
Incorporating healthy lifestyle choices, such as maintaining a balanced diet and engaging in regular physical activity, can promote joint health. Seeking medical advice for persistent symptoms can facilitate appropriate treatment and recovery.
By prioritizing joint health and addressing issues early, individuals can enjoy a more active and fulfilling life. Awareness, education, and proactive care are key components in managing joint diseases effectively.
Frequently Asked Questions
What are common joint diseases?
Common joint diseases include osteoarthritis, rheumatoid arthritis, bursitis, and tendinitis.
How can I maintain joint health?
Maintaining joint health involves regular exercise, a balanced diet, and avoiding repetitive stress on the joints.
What are the symptoms of joint diseases?
Symptoms typically include joint pain, stiffness, swelling, and limited mobility.
When should I see a doctor for joint pain?
Seek medical advice if joint pain persists, worsens, or is accompanied by swelling or deformity.
Can joint diseases be prevented?
While not all joint diseases can be prevented, maintaining a healthy lifestyle and managing risk factors can reduce the likelihood of developing them.

Zade Smith is a Proficient writer on TechsBlip, dedicated to delivering high-quality content that bridges the gap between medical research and accessible, reader-friendly guidance. With a keen interest in promoting healthy lifestyles and disease prevention, Zade’s writing offers expert insights, actionable tips, and evidence-based information to help readers make informed decisions about their health and wellness